This study was more interesting in its entirety than its abstract. I thought the home exercises given were beyond banal, but they still turned out best in the long term. Cortisone injected into tendons was yet again shown to be fool’s gold, and shock wave therapy? I don’t know but I’m still skeptical. More comments below…
Abstract
BACKGROUND:
There are no controlled studies testing the efficacy of various nonoperative strategies for treatment of greater trochanter pain syndrome. Hypothesis The null hypothesis was that local corticosteroid injection, home training, and repetitive low-energy shock wave therapy produce equivalent outcomes 4 months from baseline.STUDY DESIGN:
Randomized controlled clinical trial; Level of evidence, 2.METHODS:
Two hundred twenty-nine patients with refractory unilateral greater trochanter pain syndrome were assigned sequentially to a home training program, a single local corticosteroid injection (25 mg prednisolone), or a repetitive low-energy radial shock wave treatment. Subjects underwent outcome assessments at baseline and at 1, 4, and 15 months. Primary outcome measures were degree of recovery, measured on a 6-point Likert scale (subjects with rating completely recovered or much improved were rated as treatment success), and severity of pain over the past week (0-10 points) at 4-month follow-up.RESULTS:
One month from baseline, results after corticosteroid injection (success rate, 75%; pain rating, 2.2 points) were significantly better than those after home training (7%; 5.9 points) or shock wave therapy (13%; 5.6 points). Regarding treatment success at 4 months, radial shock wave therapy led to significantly better results (68%; 3.1 points) than did home training (41%; 5.2 points) and corticosteroid injection (51%; 4.5 points). The null hypothesis was rejected. Fifteen months from baseline, radial shock wave therapy (74%; 2.4 points) and home training (80%; 2.7 points) were significantly more successful than was corticosteroid injection (48%; 5.3 points).CONCLUSION:
The role of corticosteroid injection for greater trochanter pain syndrome needs to be reconsidered. Subjects should be properly informed about the advantages and disadvantages of the treatment options, including the economic burden. The significant short-term superiority of a single corticosteroid injection over home training and shock wave therapy declined after 1 month. Both corticosteroid injection and home training were significantly less successful than was shock wave therapy at 4-month follow-up. Corticosteroid injection was significantly less successful than was home training or shock wave therapy at 15-month follow-up.
My comments:
I found it interesting that the authors recognized that lateral hip pain, frequently diagnosed as trochanteric bursitis, rarely finds bursitis (inflamed bursa) when MRI is performed. They correctly noted that what is usually found is gluteus medius and minimus tendinopathy or tearing. The gluteus medius and minimus are hip abductors, which are the muscle you work when you lay on your side and lift your leg out Jane Fonda style. Strangely, however, in their home exercise program they didn’t do any hip abduction exercises. Rather, they did two stretches (piriformis stretch and IT band) and three quasi strength/endurance exercises, all without added resistance (straight leg raise, wall squat with ball between knees, and prone hip extension).
When I’m trying to strengthen a muscle, like almost every great athlete in the world, I prefer to lift weights. However, I understand that home exercises are used because not everyone has gym access or weights at home. The side-lying hip out (aka hip abduction exercise if you speak latin) is actually a really good exercise that can be easily performed at home. The problem with this study is that they didn’t do the side-lying hip out, or any exercise to strengthen the weakened gluteus medius/minimus that actually has the tendinopathy. So to me, the home program makes as much sense as trying to treat Achilles tendinopathy without doing a calf raise or tennis/golfer’s elbow without doing wrist or reverse wrist curls. In other words, it makes almost no sense at all. Nevertheless, the exercise group had the best long term improvement, likely because even though they didn’t target the affected muscles, and even though I think the wall squat is the worst type of squat, squats in general are great. A better program would have used free squats, progressed with weights, RDLS, hip-out AND hip-in machine, and FOR SURE side-lying hip-outs! All of which is what my upcoming paper is about.
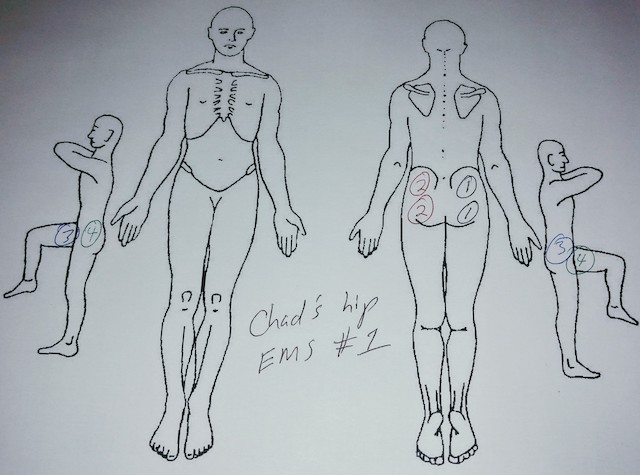
Feeling an average pain of 2.7/10 after a year isn’t ideal in my experience. With real strengthening exercises (lifting weights) combined with direct strengthening of the hip abductors (side hip outs, hip out machine, etc.) I believe patients can expect their pain to be eliminated. An aside is that in 100% of patients that I treat with greater trochanteric pain syndrome, I find their hip adductor muscles (the muscles that pull the leg back in) are also weak, making use of the hip-in machine (aka hip adduction if you speak latin) important. In general, for all tendinopathies I often find gross weakness in the general area, such that you really want a generalized strength program performed 2-3 days per week, with focused strengthening to the affected muscle performed daily. In this case I would give the side hip outs as a home exercise program. The author’s told the subjects not to expect short term improvements in pain with the exercises, but I find with targeted and more intense exercises that the pain is reduced immediately. EMS following exercise helps speed both pain reduction and strength gains along.
As has been seen with other types of tendinopathy cortisone injections start out looking great, but in the long run people who have them are worse off.
Radial shock wave therapy? I have read a few papers that say it works, but nothing yet that convinces me it works better than theatrical placebo. I’m open to hearing more about it, but the other problem is that the machines are very expensive (if I recall correctly about $150,000) and insurance won’t reimburse for treatment. I have spoken with a podiatrist that had one in his office to treat plantar fasciitis (and I have a lot to say about plantar fasciitis) for which he said he thought it worked, but said he never used it because insurance wouldn’t cover it and it was too expensive to pay out of pocket, so what good is that?
One final point of interest from this paper was that the resistance test used to diagnose GTPS was supine resisted external rotation rather than resisted abduction. I might start adding that to my evaluations when I expect GTPS as I find hip abduction is very often weak, but not that painful. I’m curious if hip external rotation more reliably reproduces symptoms of pain. If so, it would make me think my hip out machine more ideal, as I have often thought that hip abduction performed in sitting really hits the hip external rotators.
Thanks for reading my blog. If you have any questions or comments (even hostile ones) please don’t hesitate to ask/share. If you’re reading one of my older blogs, perhaps unrelated to neck or back pain, and it helps you, please remember SpineFit Yoga for you or someone you know in the future.
Chad Reilly is a Physical Therapist, obtaining his Master’s in Physical Therapy from Northern Arizona University. He graduated Summa Cum Laude with a B.S. Exercise Science also from NAU. He is a Certified Strength and Conditioning Specialist, and holds a USA Weightlifting Club Coach Certification as well as a NASM Personal Training Certificate. Chad completed Yoga Teacher Training at Sampoorna Yoga in Goa, India.

Leave a Reply